 Case Report
Case Report
A Young Lady with Unilateral Sudden Painful Complete Ophthalmoplegia: Tolosa- Hunt Syndrome
Richmond Ronald Gomes*
Professor, Medicine, Ad-din Women’s Medical College Hospital, Dhaka, Bangladesh
Richmond Ronald Gomes, Professor, Medicine, Ad-din Women’s Medical College Hospital, Dhaka Bangladesh.
Received Date:May 01, 2024; Published Date:June 10, 2024
Abstract
Tolosa–Hunt syndrome (THS) is a painful ophthalmoplegia characterized by recurrent unilateral periorbital or hemicranial pain, ipsilateral ocular motor nerve paralysis, oculosympathetic paralysis, sensory loss in the distribution of the ophthalmic and occasionally the maxillary division of the trigeminal nerve and a rapid response to steroids. Various combinations of these cranial nerve palsies may occur, localizing the pathological process to the region of the cavernous sinus/superior orbital fissure. Our report describes a 40-year-old young lady who presented with sudden, severe right hemicranial and periorbital pain with ipsilateral 3rd,4th, 6th cranial nerve palsies along with ophthalmic division of trigeminal nerve involvement. MRI of orbit showed hypo-intense lesion in right cavernous sinus extending to right superior orbital fissure (suggestive of granulomatous infiltration). THS is a diagnosis of exclusion. After taking oral steroid her pain was relieved quickly and cranial nerve palsies reversed within two weeks.
Keywords:Ophthalmoplegia; Cavernous sinus; Granulomatous infiltration; Steroid
Introduction
Painful ophthalmoplegia refers to periorbital or hemicranial pain plus ipsilateral ocular motor nerve palsies with or without oculo-sympathetic paralysis, sensory loss in the distribution of the ophthalmic and occasionally the maxillary division of the trigeminal nerve can co-occur [1]. The only anatomic locations where the ocular motor nerves, the first division of the trigeminal nerve and the internal carotid artery co-exist are the cavernous sinus and superior orbital fissure [1]. Painful ophthalmoplegia can result from neoplasic, vascular, inflammatory or infectious disease. Tolosa-Hunt syndrome (THS), a steroid-responsive painful ophthalmoplegia secondary to idiopathic, sterile, granulomatous inflammation of the cavernous sinus or orbital apex [2,3], was first described by Tolosa in 1954 [4]. In 1961, Hunt et al [5], reported six cases of painful ophthalmoplegia; that rapidly improved with the use of steroids Its pathology is described as fibroblastic, lymphocytic, and plasmacytic infiltration of the cavernous sinus. A possible risk factor for Tolosa- Hunt syndrome is a recent viral infection.THS criteria was first provided by the International Headache Society (IHS) in 1988 [6], and modified (Table 1) in the revised IHS headache classification of 2004 [7]. With no sex predilection Tolosa-Hunt syndrome can affect people of any age from 1st to 8th decades of life. THS can be classified [8], according to neuroimaging in benign (when no abnormal neuroimaging can be found), inflammatory (when inflammatory findings are shown on MRI or biopsy) and symptomatic (when neuroimaging reveals specific lesion). The characteristic findings are pain which may precede the ophthalmoplegia by several days, or may not appear until sometime later. Pain is steady, felt behind the eye often described as “gnawing” or “boring”. The neurological involvement is not confined to the third cranial nerve, but may include the fourth, sixth, and first division of the fifth cranial nerves. Periarterial sympathetic fibers and the optic nerve may also be involved. Symptoms last for days to weeks. Spontaneous remissions may occur and sometimes with residual neurological deficit. As many as 30-40% of individuals may have a relapse of Tolosa-Hunt syndrome, usually on the same side. There is no systemic reaction [9]. THS is a diagnosis of exclusion; In fact, during the initial patient evaluation there are often no clues in the history or physical examination to distinguish Tolosa-Hunt syndrome from other causes of painful ophthalmoplegia. Therefore, the clinician should be aware of causes of parasellar syndrome and other entities producing painful ophthalmoplegia. diagnostic work-up1, includes routine blood work, inflammatory markers, fasting glucose, CSF evaluation, ANA, anti-ds DNA, c-ANCA, MRI, conventional angiography or MRA. To establish the diagnosis biopsy is required through neurosurgical approach which is rarely done [10-14]. Treatment should be with high dose steroids (1 mg/kg/d) tapered slowly over 3 to 4 months [1].
Table 1:ICHD-II classification part three. Cranial neuralgias, central and primary facial pain and other headaches.
Case Report
We present the case of a 40-year-old Bangladeshi female previously healthy, whose relevant medical history only episodic bronchial asthma since childhood. The patient was admitted to our hospital for right periorbital pain, drooping of right eye lid and diplopia. Four days prior to admission, the patient started severe right periorbital pain. The pain was sudden in onset, global, continuous, associated with vomiting for several times, this relieve the headache to some extent. The following morning when she woke up from sleep, found that she cannot open her right eye voluntarily but can do manually. Her left eye was normal as well as vision. She also had horizontal diplopia on right eye. As pain did not cede after the administration of NSAID, which was the reason why the patient decided to resort to the hospital. She indicated that she had had similar episodes of headache preceded by blurring of vision in the same eye for more than a year. She denied any fever, limb weakness, convulsion, swallowing, sensory or sphincteric disturbances, joint pain, rash or any OCP use.
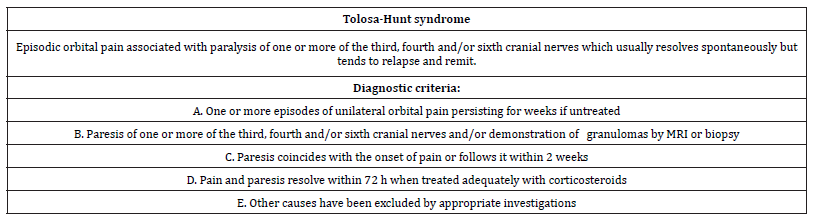
On examination, her weight 79 kg, height: 1.47 mt, 20/20 vision, normal vitals, normal fundus bilaterally, right complete ptosis, paresis of the third, fourth and sixth right cranial nerves(Figure 1), and hypoesthesia over the first division of the right trigeminal nerve. Pupil was dilated, non-reacting to light on right side. The left eye and the rest of the physical examination did not show further abnormalities (Figure 1).
Her initial laboratory tests showed white blood cell count, 9.400/ml; red blood cell count, 4.56×10/μl; hemoglobin, 13.1 g/ dl; platelets 183×103; ESR 89 mm in 1st hour. Glucose, 82 mg/dl, blood urea nitrogen, 10 mg/dl; creatinine, 0.83 mg/dl; ELISA for HIV, negative; D-Dimer, 351 ng/ml (<500 ng/ml). Thyroid function tests showed TSH, 1.81 μUI/ml (0.34-5.60); free T3, 3.64 pg/ml (2.50 - 3.90); free T4, 0.96 ng/ dl (0,54-1.64). The cerebral spinal fluid reported 4 mononuclear cell/uL; glucose, 69 mg/dl; proteins, 55 mg/dl; ADA and PCR in CFS for tuberculosis were negative. ANA was positive in cytoplasmic pattern 1:40; anti-ds DNA, ENA profile, c-ANCA and p-ANCA were negative. CT scan of brain and paranasal sinus, MRV and MRA of the brain were normal (figure 3). (SOV) thrombosis was seen. MRI of brain with orbit with contrast was done in multiple axial, coronal and sagittal sections which showed iso to hypo-intense lesion in right cavernous sinus extending up to right superior orbital fissure (figure 2). The lesion was brilliantly contrast enhancing and causing significant compression of the neurovascular structure of right cavernous sinus. Both optic nerves were spared. ICA was also normal in diameter (Figure 2 & 3).
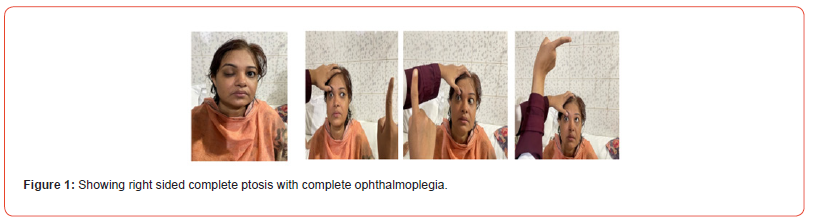
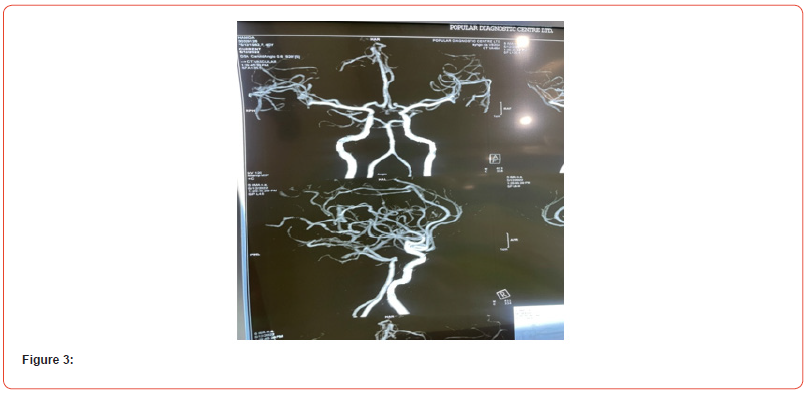
Figure 2 and figure 3 showing Axial MRI Brain T1W image reveals intense enhancement of the soft-tissue mass within the right cavernous sinus (black arrow) and normal MRA of brain respectively. Since the studies showed no abnormalities and we excluded neoplasic, infectious, vascular, thyroid and metabolic causes of painful ophthalmoplegia, we decided to start treatment for Tolosa- Hunt Syndrome with metilprednisolne 1 gr IV daily for 3 days, and noticed significant response of the right periorbital pain, palpebral ptosis and the ipsilateral ocular motor nerve palsies in next 2 weeks. At day 4, we changed treatment to prednisone at 1 mg/kg daily. Two weeks later, we initiated steroid tapering every week, and at week 12 the patient was asymptomatic and her neuro- ophthalmologic examination was completely normal.(Figure 4). The probable diagnosis of Tolosa–Hunt Syndrome was retained in the face of the negativity of all investigations carried out as well as spectacular response to treatment (Figure 4).

Discussion
Tolosa–Hunt syndrome is a painful ophthalmoplegia due to nonspecific inflammation of the cavernous sinus. Existence of this syndrome has long been debated, and its nosological framework was discussed [15]. Tolosa4 first described the condition in 1954, in a patient with unilateral recurrent painful ophthalmoplegia involving cranial nerves III, IV, VI and V1. The patient was imaged using carotid angiography and segmental narrowing of the carotid siphon was seen. Hunt et al. described 6 patients with similar clinical findings in 1961, and proposed a low-grade non-specific inflammation of the cavernous sinus and its walls as the cause of the syndrome5. Pathologically, infiltration of lymphocytes and plasma cells as well as thickening of the dura mater was seen. In 1966 Smith and Taxdal termed this condition as Tolosa-Hunt syndrome [16].
In 1988, THS criteria were provided by the International Headache Society (IHS), and further revised in 2004 (Table 1).
The etiology of Tolosa-Hunt syndrome remains unknown. No information is available as to what triggers the inflammatory process in the region of the cavernous sinus/superior orbital fissure. It seems that the syndrome falls within the range of idiopathic orbital inflammation (pseudotumour) [17]. Thus, “non-specific” inflammation typically causes an acute orbitopathy. If located more posteriorly, the inflammatory process involves the cavernous sinus/superior orbital fissure, producing the Tolosa-Hunt syndrome. Rarely, the inflammation may spread intracranially [18,19,20].
Tolosa-Hunt syndrome is caused by an inflammatory process.
Tolosa4 originally described non-specific, chronic inflammation with proliferation of fibroblasts and infiltration of the septa and wall of the cavernous sinus with lymphocytes and plasma cells. Hunt et al 5 corroborated these findings, emphasizing the lack of necrosis and pointed out that “such inflammatory changes, in a tight connective tissue, may exert pressure upon the penetrating nerves.” Subsequent reports have shown granulomatous inflammation, with epithelioid cells and occasional giant cells [6,12]. Necrosis may also be seen. There have been no reports of an infectious organism associated with Tolosa-Hunt syndrome.
Age of patients varies between 4 and 75 years 23, but THS can affect people of any age, without predominance of sex. In general, it is unilateral, but cases of bilaterality have been reported [9]. Our patient was 40 years old, and she presented with unilateral symptoms. The diagnosis of this syndrome was retained in the face of the negativity of all the investigations carried out as well as the response to treatment. Extensive diagnosis tests to exclude other common etiologies of painful ophthalmoplegia were not found in our patient.
With careful clinical examination, pain associated with typical cranial nerve palsies localizes the pathological process to the regions of the cavernous sinus/superior orbital fissure. As noted above, current neuroimaging modalities allow visualization of the area of suspected pathology. Contrast enhanced MRI with multiple views, particularly coronal sections, should be the initial diagnostic study performed. Numerous reports have demonstrated an area of abnormal soft tissue in the region of the cavernous sinus in most, but not all, patients with Tolosa-Hunt syndrome [14,24,25,26,27]. Typically, the abnormality is seen as an intermediate signal intensity on T1 and intermediate weighted images, consistent with an inflammatory process. In addition, there is enhancement of the abnormal area after intravenous injection of paramagnetic contrast. With corticosteroid therapy, the abnormal area decreases in volume and signal intensity in most reported cases.
High resolution CT can also demonstrate soft tissue changes in the region of the cavernous sinus/superior orbital fissure, but is less sensitive than MRI [2,24]. This is due to lack of sensitivity to soft tissue change with superimposed beam hardening and bone streak artifacts. Thus, even if CT is normal, MRI must still be performed to appropriately evaluate the region of the cavernous sinus or superior orbital fissure.
The major limitation of MRI findings in Tolosa-Hunt syndrome is their lack of specificity. Thus, Yousem et al 24 examined 11 patients and reported pathological MRI findings in the cavernous sinus in nine. In six of these nine the affected cavernous sinus was enlarged; in five of nine it had a convex lateral wall. Extension into the orbital apex was seen in eight patients. Yet the signal characteristics (hypointense relative to fat and isointense with muscle on T1 weighted images; isointense with fat on T2 weighted scans) were also consistent with meningioma, lymphoma, and sarcoidosis. Some authors reported that using carotid angiography there was segmental narrowing of the carotid siphon was seen [28].
Because of this fundamental limitation of initial imaging studies, some authorities would suggest that resolution of imaging abnormalities after a course of systemic corticosteroids should be considered diagnostic of THS [14,29]. However, caution is advised when assessing the salutary effects of steroids, as improvement both clinically and radiologically may occur with other disease processes.” False positive” steroid responsiveness with a “remitting” course can be seen with both malignant processes (for example, lymphoma) as well as more benign disorders (for example, vasculitis) [30].
Categorically, Tolosa-Hunt syndrome is a diagnosis of exclusion requiring careful patient evaluation to rule out tumor, vascular causes, or other forms of inflammation in the region of the cavernous sinus/superior orbital fissure. Occasional reports have documented a raised erythrocyte sedimentation rate and leukocytosis in the acute stage of Tolosa-Hunt syndrome [12,21,31,32,33]. Similarly, positive LE cell preparation and antinuclear antibody concentrations [32,34] have been documented in patients with Tolosa-Hunt syndrome, but there is no convincing evidence that such patients either have or will develop connective tissue disorder.
In general, CSF examination should also be unremarkable, although rarely raised protein and mild pleocytosis have been reported. However, if CSF abnormalities persist, the diagnosis of Tolosa- Hunt syndrome is untenable, and further diagnostic evaluations are required. As noted above, MRI is the initial diagnostic study to be performed in patients with a disorder of the cavernous sinus or superior orbital fissure. Computed tomography is a very useful adjunct in detecting bone changes (for example, erosion, hyperostosis) as well as (perisellar) calcification. Cerebral angiography has detected abnormalities in the intracavernous carotid artery in patients with Tolosa-Hunt syndrome [12,13, 21,32,35,36,37].
These have been described as “segmental narrowing”, “slight irregularity”, or “constriction”, and will resolve with corticosteroid therapy. The role of noninvasive vascular MRI techniques (MR angiography and venography) has not been defined in patients with the syndrome but these may prove to be valuable adjuncts in diagnostic evaluation.
Neurosurgical biopsy is only rarely employed to establish the diagnosis [12,13,21,22,32,35]. This can be technically difficult and should only be performed by experienced neurosurgeons. It usually involves biopsy of the dural wall of the cavernous sinus. Although generally a procedure of last resort, it should be considered in patients with rapidly progressive neurological deficits, lack of steroid responsiveness, or persistent abnormalities on neuroimaging studies.
The spectacular efficacy of corticosteroid therapy is suggestive but not specific. Hence it is necessary to conduct prolonged monitoring of several months to retain this diagnosis definitively. Treatment consists of a high dose of oral prednisone for 4 weeks. Significant improvement is often evident from the first 24 hours of treatment [38]. Our patient received a dose of prednisone 60 mg per day, and after two weeks, a complete dramatic regression of the symptoms was observed. Steroid therapy was tapered over next 4 months period. After more than six months of monitoring, no clinical abnormality was observed in our patient. Zhang et al.[15] reported that 77.5% of patients obtained complete relief of orbital pain within a week after the start of steroid treatment. This spectacular efficacy of corticosteroid therapy has been observed in several other studies [39,40,41,42].
Conclusion
Tolosa-Hunt syndrome (THS) is a rare disorder. Although the pathogenetic basis of THS remains unknown, from a practical clinical standpoint it can be regarded as a distinct entity which may be simulated by various other disorders. Tolosa-Hunt syndrome is not a fatal disorder. It remains a diagnosis of exclusion. It cannot be emphasized too strongly that patients suspected of having the syndrome require careful evaluation, appropriate treatment, and scrupulous follow up observation. We would also like to emphasize the importance of steroid treatment; even though there is no standardized dose indicated in the literature, this type of treatment with steroids at a dose of 1 mg/kg/day tapered slowly over 3 to 4 months has been well received.
Conflict of interest
None declared.
Acknowledgement
None.
References
- Gladstone JP (2007) An Approach to the Patient With Painful Ophthalmoplegia, with a Focus on Tolosa-Hunt Syndrome. Curr Pain Headache Rep 11: 317-325.
- Kwan ES, Wolpert SM, Hedges TR III, Laucella M (1988) Tolosa-Hunt syndrome revisited: not necessarily a diagnosis of exclusion. Am J Roentgenol 150: 413-418.
- Goadsby PJ, Lance JW (1989) Clinicopathological correlation in a case of painful ophthalmoplegia: Tolosa-Hunt syndrome. J Neurol Neurosurg Psychiatry 52: 1290-1293.
- Tolosa E (1954) Periarteritic lesions of the carotid siphon with the clinical features of a carotid infraclinoid aneurysm. J Neurol Neurosurg Psychiatry 17:300-302.
- Hunt WE, Meagher JN, LeFever HE, Zeman W (1961) Painful ophthalmoplegia. Its relation to indolent inflammation of the cavernous sinus. Neurology 11: 56-62.
- (1988) Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Headache Classification Committee of the International Headache Society. Cephalalgia 8: 1-96.
- Lance JW, Olesen J (2004) The International Classification of Headache Disorders ICHD-II. Cephalalgia 24: 131.
- La Mantia L, Curone M, Rapoport AM, Bussone G (2006) Tolosa-Hunt syndrome: critical literature review based on IHS 2004 criteria. Cephalalgia 26:772-781.
- L B Kline, W F Hoyt (2001) The Tolosa-Hunt syndrome.J. Neurol Neurosurg Psychiatry 71: 577–82.
- Mathew NT, Chandy J (1970) Painful ophthalmoplegia. J Neurol Sci 11:243–256.
- Aron-Rosa D, Doyon D, Sallamon G, et al. (1978) Tolosa-Hunt syndrome. Ann Ophthalmol 10:1161–1168.
- Sondheimer FK, Knapp (1973) Angiographic findings in the Tolosa-Hunt syndrome: painful ophthalmoplegia. Radiology 106:105–112.
- Hallpike J (1973) Superior orbital fissure syndrome. J Neurol Neurosurg Psychiatry 36:486–490.
- Areaya AA, Cerezal L, Canga A, et al. (1999) Neuroimaging diagnosis of Tolosa-Hunt syndrome: MRI contribution. Headache 39:321–25.
- X Zhang, Z Zhou, TJ Steiner, et al., (2014) “Validation of ICHD-3 beta diagnostic criteria for 13.7 Tolosa-Hunt syndrome:analysis of 77 cases of painful ophthalmoplegia,” Cephalalgia 34(8): 624–632.
- Smith JL, Taxdal DS (1966) Painful ophthalmoplegia. The Tolosa-Hunt syndrome. Am J Ophthalmol 61(6): 1466–1472.
- Levy IS, Wright JE, Lloyd GAS (1975) Orbital and retro-orbital pseudo-tumor. Modern Problems of Ophthalmology 14: 364-7.
- Kaye AH, Hahn JF, Craciun A, et al. (1984) Intracranial extension of inflammatory pseudotumor of the orbit. J Neurosurg 60: 625-9.
- Frohman LP, Kupersmith MJ, Lang J, et al. (1986) Intracranial extension and bone destruction in orbital pseudotumor. Arch Ophthalmol 104: 380-4.
- Bencheif B, Zovaoui A, Chedid G, et al. (1993) Intracranial extension of idiopathic orbital inflammatory pseudotumor. AJNR Am J Neuroradiol 14:181-4.
- Schatz NJ, Farmer P (1972) Tolosa-Hunt syndrome: the pathology of painful ophthalmoplegia. In: Smith JL, ed. Neuroophthalmology. Symposium of the University of Miami and the Bascom Palmer Eye Institute. Vol VI. St Louis: Mosby: 102-12.
- Aron-Rosa D, Doyon D, Sallamon G, et al. (1978) Tolosa-Hunt syndrome. Ann Ophthalmol 10:1161-8.
- Mandrioli, G. Frank, P. Sola et al. (2004) “Tolosa-hunt syndrome due to actinomycosis of the cavernous sinus: the infectious hypothesis revisited,” Headache: ,e Journal of Head and Face Pain 44(8): 806–811.
- Yousem DM, Atlas SW, Grossman RI, et al. (1990) MR imaging of Tolosa-Hunt syndrome. AJNR Am J Neuroradiol 10: 1181-4.
- Gato Y, Hosokawa S, Goto I, et al. (1990) Abnormality in the cavernous sinus in three patients with Tolosa-Hunt syndrome: MRI and CT ®ndings. J Neurol Neurosurg Psychiatry 53: 231-4.
- Desai SP, Carter J, Jinkins JR (1991) Contrast-enhanced MR imaging of Tolosa-Hunt syndrome: a case report. AJNR Am J Neuroradiol 12: 182-3.
- Obadasi Z, Gökeil Z, Atilla S, et al. (1997) The value of MRI in a case of Tolosa-Hunt syndrome. Clin Neurol Neurosurg 99:151-4.
- Som PD, Curtin HD (2003) Head and Neck Imaging. 4th ed. St Louis: Mosby: 587-591.
- Pascual J, Cerezal L, Canga A, et al. (1999) Tolosa-Hunt syndrome: focus on MRI diagnosis. Cephalgia;19(suppl 25): 36-8.
- Förderreuther S, Straube A (1999) The criteria of the International Headache Society for Tolosa-Hunt syndrome need to be revised. Neurol 246: 371-7.
- Lakke JPWF (1962) Superior orbital ®ssure syndrome. Report of a case caused by local pachymeningitis. Arch Neurol 7: 289-300.
- Mathew NT, Chandy J (1970) Painful ophthalmoplegia. J Neurol Sci 11:243-56.
- Zafrulla KM, Dhir SP, Jain IS (1977) Tolosa-Hunt syndrome. Ind J Ophthalmol 25:21-6.
- Lesser R, Jampol LM (1974) Tolosa-Hunt syndrome and antinuclear factor. Am J Ophthalmol 77: 732-4.
- Spinnler H (1973) Painful ophthalmoplegia; the Tolosa-Hunt syndrome.Med J Aust 2: 645-6.
- Julien J, Vallat JM, Vallat M, et al. (1975) Orbital phlebography in the diagnosis of painful ophthalmoplegia. Neuroradiology 9:163-6.
- Adams AH, Warner AW (1975) Painful ophthalmoplegia: report of a case with cerebral involvement and psychiatric complications. Bull Los Angeles Neurol Soc 40: 49-55.
- S Çakirer (2003) “MRI findings in Tolosa-Hunt syndrome before and after systemic corticosteroid therapy,” European Journal of Radiology 45(2): 83–90.
- V Chaudhary, S Venu, J Deswal (2016) “Painful ophthalmoplegia due to Tolosa-Hunt syndrome: a case report,” International Journal of Medical Science and Public Healthvol 5(5): 1045–1049.
- MK Singh, B Marshall, J Hawley (2014) “Painful ophthalmoplegia: a case of tolosa-hunt syndrome,” Military Medicine 179(11): e1409-e1410.
- K Okabe, R Kaneko, T Kawai, D Mochizuki, S Tsuchiya, H Hibi (2018) “Ophthalmoplegia considered to be Tolosa-Hunt syndrome: a case report,” Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology 30(5): 461–465.
- J Paovic, P Paovic, I Bojkovic, M Nagulic, V Sredovic (2012) “Tolosa-Hunt syndrome-diagnostic problem of painful ophthalmoplegia,” Vojnosanitetski Pregled 69(7): 627–630.
-
Richmond Ronald Gomes*. A Young Lady with Unilateral Sudden Painful Complete Ophthalmoplegia: Tolosa- Hunt Syndrome. Arch Neurol & Neurosci. 16(5): 2024. ANN.MS.ID.000897.
-
Acute Polyradiculoneuritis, Neurology, Guillain-barre; Fann teaching hospital, neuropathy, cranial nerves, immunotherapy, Neuroscience, neurogenic syndrome, epidemiological, Dysphonia.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






